
Truth be told: I was a fat kid. I was called names and made fun of in elementary school. It’s a painful childhood memory.
I don’t remember my parents or doctor talking to me about my weight (they may have). I do remember earning “clean plate club” honors a lot. As I was starting high school, I’d had it with shopping in the Sears section for heavy kids. I was missing out and unhappy about my weight. I didn’t lose it in the best way (I remember Tab and those old Weight Watchers chocolate squares), but did drop 25 pounds before 9th grade.
Yes, those were different times, and salt-laden casseroles and sugary Jell-O were staples at family gatherings and church dinners. At home, Durkee french fried onion rings and shoestring potato sticks in a can were always in the cupboard . . . to top off those casseroles. They were ready-to-eat bad snacks I grabbed for instant “food.”
As I got older, I learned more about unhealthy habits. Given my experience, I cringed when I read the latest stats from the Centers for Disease Control and Prevention: more than one third of U.S. children and teens are overweight or obese, and obesity has doubled in children and quadrupled in adolescents over the last 30 years!
Sadly, a New England Journal of Medicine article says the road to obesity starts before age 5.
Childhood obesity is more upsetting because the extra pounds often start kids on the path to health problems that were once only adult issues, like diabetes, high blood pressure and high cholesterol. And as I know, it can also affect self-esteem.
How can we help our kids?
It may come as no surprise that new guidelines published last Monday, June 29, by the American Academy of Pediatrics say we need to focus on prevention.
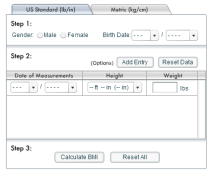
This starts by understanding when a child is considered obese—when a child is well above the normal weight for his or her age and height, as measured by body mass index (BMI). The standards are:
- Overweight = BMI-for-age between 85th and 94th percentiles
- Obese = BMI-for-age 95th percentile or above
(You can use this tool from Kid’s Health to check your children.)
Make better food choices and exercise
 One of the best strategies to prevent childhood obesity is to lead by example, improving diet and exercise habits of your whole family.
One of the best strategies to prevent childhood obesity is to lead by example, improving diet and exercise habits of your whole family.
Most of us know to buy fewer sweetened beverages (sodas, juice and sports drinks) and not stock junk food in the house (or buy it in bulk!). We’ve also heard about First Lady Michelle Obama’s Let’s Move initiative stressing physical activity and the recommended 60 minutes of active play time day.
So how do we put good habits into practice? A few practical tips:
- Don’t ban junk food outright. Instead, limit the number of treats kids are allowed to eat. That way, kids aren’t as tempted to want what they can’t have or overeat when it’s offered by someone else.
- Keep fresh fruit in reach to grab as a quick snack. Put higher-calorie foods in the back of the frig or pantry. Get good frozen and canned fruits and vegetables (no and no sugar or salt) when fresh isn’t available.
-
via LetsMove.org Make an effort to limit technology time for kids to no more than 2 hours a day, including computers, videos, games, watching TV. Turn off the TV during family meals to prevent distracted eating (and more) – Have you seen Dixie’s Dark for Dinner ads?
- Plan activities that give everyone exercise, like walking, biking and swimming. Turn a walk after dinner into a family affair.
- Make sure your kids get enough sleep, since studies suggest there’s a link between obesity and insufficient sleep.
For more: check out these 10 healthy eating tips and take advantage of the thousands of healthy MyPlate recipes on Pinterest.
Physician education
We now know doctors have to get more involved. While weight is an uncomfortable and awkward topic to tackle, physicians need to address it during children’s visits.
 Recent collaborative research between Caroline Shue, associate professor of communication studies at Ball State University and the IU Health Ball Memorial Hospital Family Medicine Residency Center found a hesitancy to discuss weight is compounded by a disconnect with the reason for the visit (e.g., an ear infection for a “solid” child) as well as a lack of doctors’ training and consistent clinic practices to calculate BMI and chart discussions with patients.
Recent collaborative research between Caroline Shue, associate professor of communication studies at Ball State University and the IU Health Ball Memorial Hospital Family Medicine Residency Center found a hesitancy to discuss weight is compounded by a disconnect with the reason for the visit (e.g., an ear infection for a “solid” child) as well as a lack of doctors’ training and consistent clinic practices to calculate BMI and chart discussions with patients.
The research identified several good ways to fix the problems, including: targeted training programs for doctors; and doctor’s offices documenting patients’ height, weight, and BMI more frequently and regularly.
Support nonprofits making a difference
We can all help charities working to get kids more active and prevent obesity. Here are three with programs designed to do just that, operating across the country:
American Heart Association

Boys & Girls Clubs of America

YMCA of the USA

We’ve come a long way since I was a little girl, and I’m encouraged by all the attention, education and resources that exist now. Let’s step up, so other kids can skip all the bad stuff that comes from carrying too much weight. Here’s to preventing childhood obesity, and raising healthier future generations!
– Candy Culver
Marketing Consultant
